Dark Spots vs Age Spots - What’s the Difference?
3 min read
The Skin's Color Story
Your skin's color comes from melanin, a pigment produced by cells called melanocytes. When these cells produce too much melanin in certain areas, you get darker patches - what we call hyperpigmentation. While the terms "dark spots" and "age spots" are often used interchangeably, they represent different types of skin discoloration with distinct causes and characteristics.
Age Spots - The Sun's Signature
Age spots (also called liver spots, solar lentigines, or sun spots) are light brown or gray spots on your skin that result from years of sun exposure. Despite their name, age spots aren't caused by aging itself - they're caused by cumulative sun damage over time.
Key Characteristics:
Flat, brown or gray patches
Well-defined borders
Most commonly appear on sun-exposed areas like hands and face
Typically range from freckle-size to about 1/2 inch across
More common after age 40, but can appear earlier with significant sun exposure
What Happens in Your Skin - When UV rays hit your skin repeatedly over years, melanocytes (pigment-producing cells) go into overdrive. They create clusters of excess melanin as your skin's attempt to protect itself from further damage. Think of age spots as your skin's "memory" of past sun exposure.
Dark Spots - The Broader Category
Dark spots encompass several types of hyperpigmentation beyond age spots:
Post-Inflammatory Hyperpigmentation (PIH)
Darkening of the skin in an area of prior injury or inflammation
Significantly more common and severe in darker skin types (affecting 65.3% of African-Americans, 52.7% of Hispanics, and 47.4% of Asians after acne)
Triggered by acne, cuts, burns, eczema, or even harsh skincare treatments
Can appear anywhere on the body, regardless of sun exposure
Melasma
Chronic skin condition marked by dark brown or gray patches of discoloration
Often called "pregnancy mask" due to hormonal triggers
Typically appears on the face in symmetric patterns
More common in women (19:1 female-to-male ratio, approximately 95% female)
Worsened by sun exposure and hormonal changes
Prevention - Your First Line of Defense
Sun Protection (Critical for All Types):
Use broad-spectrum SPF 30+ sunscreen daily, rain or shine
Reapply every 2 hours when outdoors
Wear protective clothing and wide-brimmed hats
Seek shade during peak UV hours (10 AM - 4 PM)
Gentle Skincare Practices:
Avoid picking at acne or wounds (prevents PIH)
Use gentle, non-irritating skincare products
Treat inflammatory conditions promptly
Be cautious with aggressive treatments that might cause irritation
Hormonal Considerations:
Discuss alternatives if hormonal birth control triggers melasma
Extra sun protection during pregnancy
Consider timing of cosmetic procedures around hormonal changes
Treatment Options - From Gentle to Intensive
Over-the-Counter Options:
Vitamin C serums (antioxidant protection and mild lightening)
Retinol products (accelerate cell turnover)
Niacinamide (reduces inflammation and melanin transfer)
Fade creams and lotions may improve appearance, though you might need several weeks or months of regular use
Professional Treatments:
Topical Prescriptions:
Hydroquinone 4% (gold standard for lightening)
Tretinoin (prescription retinoid for faster cell turnover)
Kojic acid, azelaic acid, or arbutin (alternative lightening agents)
Combination treatments with hydroquinone and retinoids often work best
In-Office Procedures:
Chemical peels (remove damaged surface layers)
Laser treatments (target melanin deposits)
Intense pulsed light (IPL) therapy
Microdermabrasion (physical exfoliation)
Treatment Timeline Reality Check. The healing process can take months to years, necessitating prolonged treatment. Most patients see initial improvements in 6-12 weeks, but complete resolution may take 6-18 months with consistent treatment.
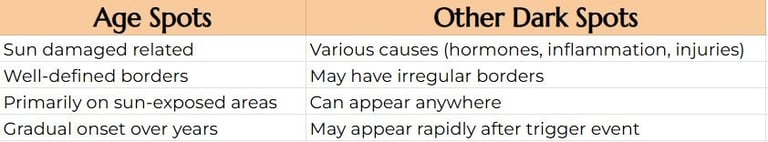
Key Differences to Remember
When to See a Dermatologist
Red Flags - Seek Immediate Evaluation
Spots that are black or have changed in appearance, as these can be signs of melanoma
Spots that are increasing in size or have irregular borders
Any new or changing pigmented lesions
Spots that bleed, itch, or become raised
Professional Treatment Candidates
Multiple or large spots affecting quality of life
Over-the-counter treatments haven't worked after 3-4 months
Suspicion of melasma (requires specialized treatment approach)
History of skin cancer or unusual moles
In Conclusion
Both age spots and other dark spots are generally benign but can significantly impact confidence and appearance. Prevention is key to limiting early signs of age spots, with consistent sun protection being your most powerful tool. While you may be able to fade spots significantly and sometimes even get rid of them, success requires patience, consistency, and often professional guidance.
Remember: not all dark spots are created equal. What works for sun-induced age spots may not be appropriate for hormonally-driven melasma. Proper diagnosis is crucial, as melasma cannot be treated with lasers designed for other forms of hyperpigmentation. When in doubt, consult a board-certified dermatologist for proper evaluation and personalized treatment planning.
The key to success lies in understanding your specific type of hyperpigmentation, committing to rigorous sun protection, and working with a dermatologist to develop a comprehensive treatment plan tailored to your skin's unique needs. Recent research shows that dyschromias like PIH are among the most common reasons darker racial/ethnic groups seek dermatological care, highlighting the importance of culturally competent treatment approaches.